Parkinson’s disease (PD) has long been a clinical enigma, a condition diagnosed not by a definitive test but by the slow, often subtle emergence of motor symptoms like tremors and rigidity. By the time a diagnosis is made, a significant portion of the brain’s critical dopamine-producing cells have already been lost. This diagnostic delay represents a major barrier to developing treatments that could slow or halt the disease’s progression. For the millions affected worldwide, a number that the World Health Organization estimated at over 8.5 million in 2019, this reality is a source of profound uncertainty.
The scientific community is now on the brink of a paradigm shift, moving away from symptom-based diagnosis towards a future defined by biological precision. This revolution is being driven by the relentless pursuit of biomarkers—objective, measurable indicators that can detect the disease at its earliest stages, track its progression, and even predict its course. These molecular and imaging signposts are illuminating the hidden pathology of Parkinson’s, offering a new language to understand this complex neurodegenerative disorder. This guide will decode that language, exploring the landscape of current and emerging biomarkers that hold the promise of transforming how we diagnose, manage, and ultimately treat Parkinson’s disease.
Introduction: Illuminating Parkinson’s Disease and the Promise of Biomarkers
Understanding Parkinson’s Disease: A Brief Overview
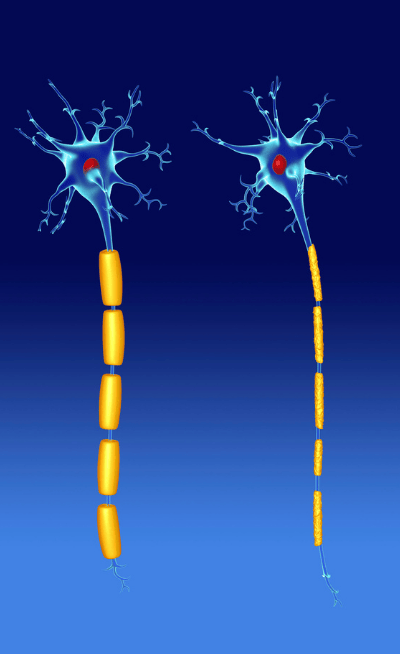
Parkinson’s disease is a progressive neurodegenerative disorder characterized primarily by the loss of dopaminergic neurons—specialized brain cells that produce dopamine—in a region of the midbrain called the substantia nigra. Dopamine is a neurotransmitter essential for controlling movement, and its depletion leads to the hallmark motor symptoms of PD: tremors, bradykinesia (slowness of movement), rigidity, and postural instability.
However, the pathology of PD extends far beyond the dopaminergic system. A key molecular event is the misfolding and aggregation of a protein called alpha-synuclein (often abbreviated as α-synuclein). In its healthy state, α-synuclein is thought to play a role in synaptic function. In PD, it clumps together to form insoluble fibrils, which are the primary component of microscopic structures called Lewy bodies. These Lewy bodies are found within surviving neurons and are considered a pathological hallmark of the disease, contributing to cellular dysfunction and eventual death. This process of neurodegeneration is not confined to the substantia nigra, affecting other brain regions and leading to a wide range of non-motor symptoms, including cognitive impairment, sleep disorders, and depression.
The Critical Need for Biomarkers in PD Management
The traditional diagnosis of Parkinson’s disease relies on a neurologist’s clinical assessment of motor symptoms, a method that is inherently subjective and can only confirm the disease after significant neurodegeneration has already occurred. This “wait-and-see” approach is a major obstacle for modern medicine. The development of neuroprotective or disease-modifying therapies hinges on our ability to intervene early, well before irreversible damage is done.
This is where the critical need for biomarkers emerges. A reliable biomarker could provide an objective, biological signature of the disease, enabling early diagnosis—potentially years before the first tremor appears. Furthermore, biomarkers could help stratify patients into different subgroups, track disease progression with greater accuracy than clinical scales, and provide definitive endpoints to measure the effectiveness of new treatments in clinical trials. They represent the essential tools needed to move from managing symptoms to fundamentally altering the course of Parkinson’s disease. The urgency is underscored by projections that the number of people with Parkinson’s worldwide could double to 25 million by 2050, creating an immense global health challenge.
The Foundation: What Are Biomarkers and Why Are They Essential for Parkinson’s?
Defining a Biomarker: Types and Utility
A biomarker, or biological marker, is a characteristic that can be objectively measured and evaluated as an indicator of a normal biological process, a pathogenic process, or a pharmacological response to a therapeutic intervention. In essence, it is a biological clue that provides a window into a person’s health status. Biomarkers can be categorized in several ways:
- Diagnostic Biomarkers: Used to detect or confirm the presence of a disease, often distinguishing it from other conditions.
- Prognostic Biomarkers: Provide information about the likely course of a disease in an individual, such as the rate of progression.
- Predictive Biomarkers: Help predict which patients are most likely to respond to a specific treatment.
- Pharmacodynamic/Response Biomarkers: Show that a biological response has occurred in a patient receiving a therapy.
- Monitoring Biomarkers: Used to track the status of a disease or the effect of a treatment over time.
For a complex condition like Parkinson’s, a single biomarker is unlikely to fulfill all these roles. Instead, the field is moving towards a panel of biomarkers, combining different types of biological information to create a comprehensive picture of an individual’s disease state.
The Role of Biomarkers in the Parkinson’s Journey
Biomarkers have the potential to revolutionize every stage of the Parkinson’s journey. For individuals at high risk due to genetics or other factors, a biomarker could signal the very beginning of the disease process, creating an opportunity for preventative strategies. For those with early, ambiguous symptoms, a diagnostic biomarker could provide a definitive and timely diagnosis, ending a period of uncertainty and allowing for earlier initiation of supportive care.
Once diagnosed, prognostic and monitoring biomarkers could help clinicians tailor treatment plans to an individual’s specific disease trajectory. Perhaps most importantly, biomarkers are indispensable for advancing research. In clinical trials for new therapies, they can help select the right patient populations (e.g., those in the earliest stages) and provide objective measures of whether a drug is successfully targeting the underlying pathology of neurodegeneration. This accelerates the development pipeline, bringing promising treatments from the lab to patients faster.
Current Challenges in Parkinson’s Diagnosis and Monitoring
The current “gold standard” for Parkinson’s diagnosis remains the clinical examination by a movement disorder specialist. While accurate in experienced hands, misdiagnosis rates can be significant, especially in the early stages when symptoms overlap with other conditions like essential tremor or atypical parkinsonian syndromes. This diagnostic uncertainty complicates patient care and muddies the waters for clinical research.
Monitoring disease progression is equally challenging. Clinicians rely on standardized rating scales, which involve subjective assessments of motor and non-motor function. These scales can be influenced by the time of day, medication effects, and patient-reported symptoms, leading to variability. The lack of objective measures makes it difficult to definitively determine if a patient’s condition is worsening slowly or rapidly, or if a new therapy is having a meaningful biological effect beyond simple symptom relief. The development of robust biomarkers is the only way to overcome these fundamental limitations and usher in an era of precision medicine for Parkinson’s disease.
Current and Established Biomarkers: Tools in Practice Today
While the quest for the perfect PD biomarker continues, several tools are already in clinical use, providing valuable, albeit incomplete, insights into the disease process. These established biomarkers fall primarily into two categories: fluid-based and imaging-based.
Fluid Biomarkers: Unlocking Insights from Bodily Fluids
Fluid biomarkers involve the analysis of biological fluids, most commonly cerebrospinal fluid (CSF) and blood, to detect molecules that reflect the underlying pathology of Parkinson’s.
Cerebrospinal Fluid (CSF): CSF, the clear fluid that bathes the brain and spinal cord, provides the most direct window into the biochemistry of the central nervous system. For years, researchers have studied proteins in the CSF of PD patients. Key findings include:
- Total and Oligomeric α-synuclein: Studies have consistently shown that, paradoxically, levels of total α-synuclein in the CSF are often lower in individuals with Parkinson’s compared to healthy controls. This is thought to be because the protein is being sequestered into Lewy bodies within the brain, reducing its concentration in the surrounding fluid.
- Other Neurodegenerative Markers: Levels of proteins like amyloid-beta 42 (Aβ42) and tau, which are primary biomarkers for Alzheimer’s disease, are also altered in PD, often reflecting the degree of cognitive impairment.
The major limitation of CSF analysis is its invasive nature, requiring a lumbar puncture (spinal tap), which is not ideal for routine screening or monitoring.
Blood-based Markers: The ultimate goal for a fluid biomarker is a simple blood test. However, this has proven exceptionally challenging. The brain is protected by the blood-brain barrier, which limits the passage of brain-derived proteins into the peripheral circulation. Furthermore, proteins like α-synuclein are also produced by cells outside the brain, such as red blood cells, creating a high level of background noise that can obscure the brain-specific signal. For these reasons, while intensely researched, a reliable blood or plasma biomarker for routine clinical use has remained elusive until very recently.
Imaging Biomarkers: Visualizing Brain Changes
Neuroimaging provides a non-invasive way to visualize the structural and functional changes occurring in the brain of a person with Parkinson’s. The most established imaging biomarker targets the hallmark dopaminergic deficit.
Dopamine Transporter (DAT) Imaging: This technique, most commonly performed using Single-Photon Emission Computed Tomography (SPECT), is known as DAT-SPECT or DaTscan. It uses a radiotracer that binds to the dopamine transporter, a protein densely packed on the terminals of dopaminergic neurons in the striatum (a brain region that receives signals from the substantia nigra).
In a healthy brain, the scan shows two bright, comma-shaped signals. In a person with Parkinson’s, the loss of dopaminergic neurons leads to a reduced signal, particularly in a part of the striatum called the putamen. The comma shape degrades into a period-like shape. DAT-SPECT is highly effective at distinguishing parkinsonian syndromes from conditions that do not involve a loss of dopamine neurons, such as essential tremor. However, it cannot differentiate Parkinson’s disease from other atypical parkinsonian disorders that also feature dopaminergic loss. While it confirms a dopamine deficit, it doesn’t reveal the underlying cause, such as the presence of α-synuclein pathology.
Emerging Biomarkers: Pioneering the Future of Parkinson’s Detection and Treatment
The field of Parkinson’s research is experiencing an unprecedented surge in biomarker discovery, driven by technological advancements and a deeper understanding of the disease’s molecular underpinnings. These emerging biomarkers promise to overcome the limitations of current tools and provide a far more detailed and accurate picture of PD.
Advanced Alpha-Synuclein Detection: A Game Changer
The central role of misfolded α-synuclein in PD pathology makes it the most sought-after biomarker target. The challenge has been to develop assays sensitive enough to detect the tiny quantities of the pathological, aggregated form of the protein amidst an abundance of its normal, healthy form. A breakthrough technology known as “seeding aggregation assays” has overcome this hurdle.
The most prominent of these is the α-synuclein Seed Amplification Assay (α-syn SAA), also known as Real-Time Quaking-Induced Conversion (RT-QuIC). This technique works by taking a small sample of a patient’s biological fluid (initially CSF, but now also blood and even skin tissue) and adding it to a solution containing a large amount of normal, recombinant α-synuclein. If even minuscule amounts of misfolded “seed” protein are present in the patient’s sample, they will trigger a chain reaction, causing the normal protein to misfold and aggregate rapidly. This amplification process can be monitored in real-time using a fluorescent dye.
The α-syn SAA has demonstrated remarkable accuracy, with studies showing over 90% sensitivity and specificity for detecting the synuclein pathology that defines Parkinson’s disease and related disorders. It is poised to become the first definitive biochemical test for PD, capable of confirming the presence of Lewy body pathology in living individuals.
Genetic and Epigenetic Biomarkers: Unraveling Inherited and Acquired Risk
While most cases of Parkinson’s are idiopathic (of unknown cause), genetics play a significant role. Mutations in genes such as SNCA (which codes for α-synuclein), LRRK2, and GBA are known to substantially increase the risk of developing PD. Genetic testing can identify these high-risk individuals, serving as a crucial risk biomarker. This is particularly important for enrolling individuals in clinical trials for preventative therapies. New research suggests that approximately 13% of people with PD have a genetic variant, a higher percentage than previously thought.
Beyond the fixed genetic code, epigenetic markers—chemical modifications to DNA that regulate gene activity without changing the DNA sequence itself—are also being explored. These markers, such as DNA methylation patterns, can be influenced by environmental factors and may provide insights into why some individuals with a genetic predisposition develop the disease while others do not.
Neuroinflammation and Immune System Markers: Tracking the Brain’s Immune Response
Neuroinflammation is increasingly recognized as a key contributor to the progression of neurodegeneration in Parkinson’s disease. The presence of misfolded α-synuclein and dying neurons activates the brain’s resident immune cells (microglia and astrocytes), triggering a chronic inflammatory response that can cause further damage to surrounding neurons.
Biomarkers that reflect this inflammatory process are gaining significant attention. One of the most promising is Glial Fibrillary Acidic Protein (GFAP), a protein released by activated astrocytes. Elevated levels of GFAP have been detected in the blood and CSF of individuals with various neurological disorders, including PD. As a marker of astrocytic activation, GFAP could serve as a valuable indicator of ongoing neuroinflammation, potentially helping to track disease activity and the response to anti-inflammatory therapies in future trials.
Other Promising Fluid Biomarkers
Beyond α-synuclein and inflammatory markers, researchers are using advanced proteomic and metabolomic techniques to search for other molecules in the blood and CSF that could serve as biomarkers. Recent landmark research has identified a panel of eight proteins in the blood that, when analyzed using machine learning algorithms, can predict the future onset of Parkinson’s disease with high accuracy up to seven years before motor symptoms appear. This panel includes proteins involved in inflammation, coagulation, and protein-misfolding response pathways.
Other potential markers under investigation include neurofilament light chain (NfL), a general marker of neuronal damage, and specific lipids and metabolites whose levels are altered by the metabolic dysfunction that occurs in PD. This multi-faceted approach aims to capture different aspects of the disease process simultaneously. The growing interest in this area is reflected in market trends, with the global blood-based biomarker for Parkinson’s disease market projected to grow from USD 117.79 million in 2024 to over USD 350 million by 2033.
Digital Biomarkers and Wearable Technology: Real-World Monitoring
The digital revolution is also transforming biomarker discovery. Digital biomarkers are objective, quantifiable physiological and behavioral data collected by digital devices such as sensors, wearables, and smartphones. For Parkinson’s, this is a particularly exciting frontier.
Wearable sensors can continuously and passively monitor motor function in a patient’s own environment, capturing subtle changes in gait, tremor, and activity levels that are impossible to assess during a brief clinical visit. Smartphone apps can measure voice changes, tapping speed, and reaction time. This wealth of real-world data can provide a highly granular and objective measure of disease progression and response to medication. The rapid growth of the broader digital health in neurology market, expected to reach over $55 billion in 2025, highlights the immense potential of these technologies.
The Power of Integration: Multi-Modal and Synergistic Biomarker Approaches
The future of Parkinson’s diagnosis and management will not rely on a single “magic bullet” biomarker. The disease is far too complex, affecting multiple biological systems. Instead, the greatest power lies in integrating information from different types of biomarkers—fluid, imaging, genetic, and digital—to create a comprehensive and personalized profile of each patient’s disease.
Combining Biomarkers for Enhanced Accuracy
A multi-modal approach can overcome the limitations of any single biomarker. For example, an α-synuclein seed amplification assay from a blood test could confirm the presence of the core pathology. A DAT-SPECT scan could then quantify the degree of dopaminergic neuron loss, providing a measure of disease stage. A blood test for GFAP or other inflammatory markers could indicate the level of ongoing neuroinflammation, offering prognostic information about the potential rate of progression.
Simultaneously, data from a wearable sensor could provide a continuous, real-world assessment of motor symptom severity. By combining these layers of information, clinicians can achieve a much higher degree of diagnostic certainty and gain a deeper understanding of the specific pathological processes driving an individual’s disease, paving the way for more targeted and effective treatments.
The Role of Artificial Intelligence and Machine Learning in Biomarker Discovery
The sheer volume and complexity of data generated by multi-modal biomarker approaches require sophisticated analytical tools. Artificial intelligence (AI) and machine learning (ML) are essential for this task. ML algorithms can analyze vast datasets, identifying subtle patterns and correlations that are invisible to human analysis.
This is precisely how the aforementioned 8-protein panel for predicting PD was discovered. Researchers fed proteomic data from thousands of plasma samples into an ML model, which learned to recognize the specific protein signature that preceded a Parkinson’s diagnosis. AI is also being used to analyze neuroimaging data, automatically quantifying changes in brain structure and function, and to interpret the complex data streams from digital health devices. AI is not just a tool for analyzing biomarkers; it is a critical engine for discovering new ones.
Towards Personalized Medicine in Parkinson’s Disease
The ultimate goal of integrating biomarkers is to enable personalized medicine. Parkinson’s is not a monolithic entity; it is a heterogeneous condition with significant variability in symptoms, progression rates, and underlying biology from one person to the next. A one-size-fits-all approach to treatment is therefore suboptimal.
By using a panel of biomarkers, it may become possible to subtype patients based on their biological profiles. For example, a patient with a strong genetic component and high levels of neuroinflammation might be a prime candidate for a gene therapy or an anti-inflammatory drug being tested in a clinical trial. Another patient with a different profile might benefit more from a therapy targeting α-synuclein clearance. This tailored approach, guided by objective biological data, holds the key to developing truly disease-modifying therapies and improving outcomes for everyone living with Parkinson’s.
Challenges, Opportunities, and the Path Forward
While the future of Parkinson’s biomarkers is incredibly bright, the path from a promising research finding to a widely available clinical tool is fraught with challenges. Overcoming these hurdles is essential to realize the full potential of these transformative technologies.
Standardization, Reproducibility, and Clinical Validation
For any biomarker to be clinically useful, the test must be reliable and reproducible. This means that a sample tested in a lab in one city should yield the same result as the same sample tested in another lab across the country. This requires rigorous standardization of laboratory procedures, from sample collection and processing to the specific reagents and equipment used in the assay.
Furthermore, every new biomarker must undergo extensive clinical validation in large, diverse patient populations. It must be proven to be not only analytically sound but also clinically meaningful. Researchers must demonstrate that the biomarker can accurately diagnose the disease, distinguish it from other conditions, and provide valuable information about prognosis or treatment response. This validation process is time-consuming and expensive but absolutely critical for regulatory approval and clinical adoption.
The Translation Gap: From Lab to Clinic
A significant challenge in medical research is the “translation gap”—the difficulty in translating exciting discoveries from the research laboratory into routine clinical practice. Even after a biomarker has been validated, logistical and economic barriers can slow its adoption. New tests must be integrated into existing clinical workflows, clinicians need to be educated on their proper use and interpretation, and healthcare systems and insurers must be convinced of their cost-effectiveness.
Closing this gap requires collaboration between academic researchers, biotechnology companies, regulatory agencies, clinicians, and patient advocacy groups. Streamlining the validation and approval processes while ensuring patient safety is a key priority for the entire Parkinson’s community.
Biomarkers for Monitoring Treatment Response and Guiding Clinical Trials
One of the most profound opportunities for biomarkers is in revolutionizing the design and execution of clinical trials. Developing new therapies for neurodegenerative diseases is notoriously difficult, in part because of the long duration of the trials and the reliance on subjective clinical endpoints. The growth of the Parkinson’s disease therapeutics market, predicted to reach USD 13.34 billion by 2034, highlights the massive investment in this area.
Biomarkers can make these trials more efficient and more likely to succeed. A diagnostic biomarker, such as the α-syn SAA, ensures that only individuals who truly have the underlying pathology of PD are enrolled, preventing the inclusion of patients with other conditions that could confound the results. Prognostic biomarkers can help select patients who are likely to progress more rapidly, allowing researchers to see a treatment effect in a shorter timeframe. Finally, pharmacodynamic biomarkers can provide early evidence that a drug is engaging its target, allowing for quicker decisions about whether to continue developing a promising therapy.